 Researchers at the University of Illinois at Chicago are the first to use brain imaging to examine the effects of emotion on working memory function in children with pediatric bipolar disorder (PBD) or attention deficit hyperactivity disorder (ADHD). PBD and ADHD are very severe developmental disorders that share behavioral characteristics such as impulsivity, irritability, and attention problems. The study is published in the October issue of the Journal of the American Academy of Child & Adolescent Psychiatry.
Researchers at the University of Illinois at Chicago are the first to use brain imaging to examine the effects of emotion on working memory function in children with pediatric bipolar disorder (PBD) or attention deficit hyperactivity disorder (ADHD). PBD and ADHD are very severe developmental disorders that share behavioral characteristics such as impulsivity, irritability, and attention problems. The study is published in the October issue of the Journal of the American Academy of Child & Adolescent Psychiatry.
Using functional magnetic resonance imaging, researchers at UIC examined the brain activity of children as they performed a working memory task while viewing faces with different emotions, such as angry, happy, or neutral expressions.
The children, ages 10 to 18, were asked to remember the faces and to press a button in the MRI-scanner if they saw the same face that was presented two trials earlier. The study involved 23 non-medicated children with bipolar disorder, 14 non-medicated children with ADHD, and 19 healthy controls.
“It’s a simple yet elegant working memory test that tells us a lot about how their brain remembers stimuli like faces or objects,” said Alessandra Passarotti, assistant professor of psychiatry at UIC and lead author of the study. “We also added in an emotional component – because both disorders show emotional deficits – to study how their working memory is affected by emotional challenge.”
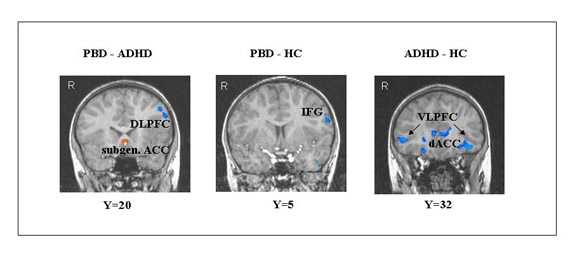
The recent brain imaging study (Passarotti, Sweeney and Pavuluri, 2010) was the first to differentiate brain dysfunction in adolescents with pediatric bipolar disorder (PBD) and attention-deficit hyperactivity disorder (ADHD) during an affective working memory task with emotional challenge. While relative to healthy peers both the PBD and ADHD group exhibited working memory deficits and dysfunction of the dorsal and ventral prefrontal cortex, important brain regions specialized for working memory and emotion regulation, the ADHD group exhibited the most severe dysfunction. Moreover, PBD relative to ADHD exhibited greater dysfunction of affect circuits whereas ADHD relative to PBD showed greater dysfunction of working memory circuits. In fig 2a, red clusters in the brain picture indicate greater brain activation in the first group compared to the second group of the comparison. Blue clusters indicate less activation in the first group compared to the second group. (DLPFC= dorsolateral prefrontal cortex; IFG=inferior frontal gyrus, VLPFC= ventrolateral prefrontal cortex; ACC=anterior cingulate cortex).
The researchers found that while both disorders show dysfunction in the prefrontal cortex relative to healthy controls, the ADHD group had the most severe dysfunction in this important region. The prefrontal cortex controls behavior, such as impulsivity, and executive function, as well as complex cognitive processes such as working memory, attention, and language.
From a treatment, learning and intervention perspective, the next step for researchers and clinicians is to figure out how to help patients use their prefrontal cortex, Passarotti said.
The researchers also found that while the ADHD group had greater dysfunction in working memory circuits in the brain, the bipolar group had more deficits in regions of the brain involved in emotion-processing and regulation.
Now that researchers are starting to differentiate between the two disorders at a brain network level, rather than just at a behavioral level, the long-term goal is to develop diagnostic tests based on neurological and behavioral markers of illness that can be used in a clinical setting. Currently patients are diagnosed using clinical measures, questionnaires, behavior scales and interviews with parents.
It is difficult for physicians to differentiate between the two disorders behaviorally, which may lead to an incorrect diagnosis and wrong medications, a worsening of symptoms, and greater frustration for children and parents, said Passarotti, a researcher in UIC’s Institute for Juvenile Research.
She said that while researchers still do not understand all of the neurological deficits that characterize ADHD and PBD profiles, they know that drug treatment that works for ADHD does not work for bipolar disorder.
“In fact, if you give a stimulant to a child with bipolar disorder, they become more manic, and this makes their illness even worse, whereas if you give the mood-regulation medicine commonly prescribed for PBD to a child with ADHD, they still show a lot of attention deficits and do not show any improvement,” Passarotti said.
“Our hope is that by better differentiating between these two severe developmental illnesses, we can help develop more accurate diagnoses and more targeted treatments for PBD and ADHD.”
Material adapted from University of Illinois at Chicago.
No comments yet.